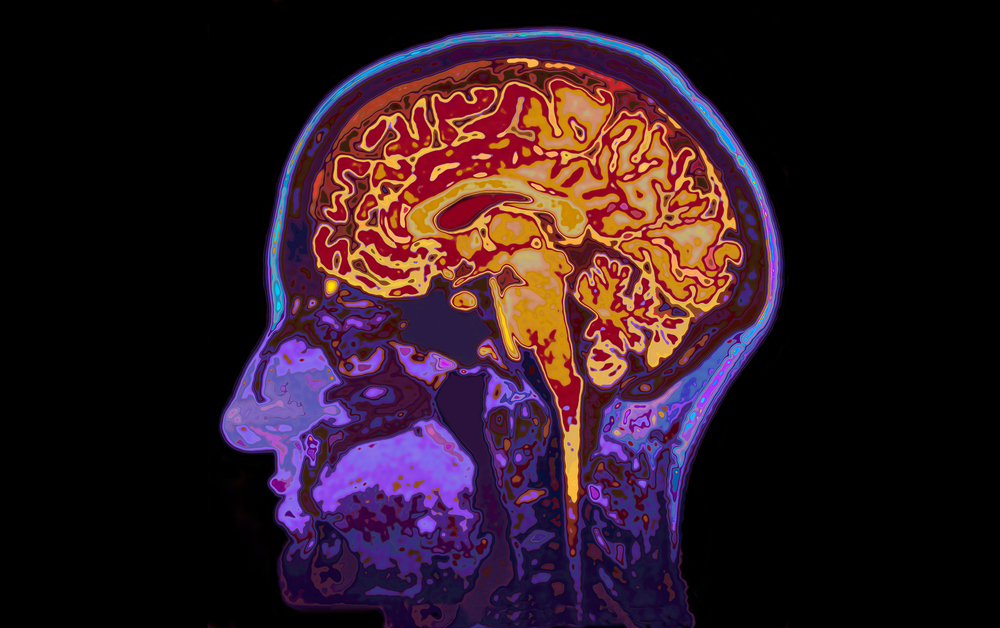
In a major step toward predicting dementia before its debilitating symptoms appear, researchers revealed an MRI ‘signature’ that could act as a warning, pinpointing the risk of getting the disease five to 10 years in advance. This unique biomarker not only offers early detection but also opens the door to treatment therapies that could potentially slow the evolution of this widespread ailment.
Decoding the silent threat: how brain MRIs hold the key
Dementia, a silent disease that is becoming more prevalent as the world’s population ages, has prompted researchers to look for early detection methods. Researchers are examining the complex realm of brain MRIs, comparing scans from people with and without dementia. The goal is to discover a distinct ‘signature’ that could signal the danger of dementia long before symptoms appear.
Early detection is critical: a global dementia initiative
With an aging global population, the need to address dementia’s public health impact has never been greater. Alzheimer’s disease, the most common type of dementia, drives a never-ending search for remedies. Early detection appears as a critical technique, creating a window of opportunity for therapeutic interventions and lifestyle changes.
Researchers at the University of Texas Health Science Center at San Antonio, in collaboration with UC Davis and Boston University, conducted a thorough investigation. They analyzed hundreds of brain MRIs to find a reliable dementia biomarker that could be applied to huge populations, providing hope for early detection and focused treatments.
The cortex connection
The researchers investigated the brain’s complexity, namely the thickness of gray matter in the cortex. The outer layer of the brain, which is rich in gray matter, is a mosaic of functional areas that control memory, reasoning, senses, and language. The findings revealed a consistent pattern: bigger ribbons were associated with a lower incidence of dementia, whereas thinner ribbons indicated a higher risk.
Consistent findings across demographics: A universal approach to dementia risk
Importantly, these insights transcended demographic distinctions. Whether in the ethnically varied Californian group or the primarily non-Hispanic white Massachusetts cohort, the relationship between cortical thickness and dementia risk was consistent. A potential universal application raises hopes for a uniform method for dementia prediction.
Breaking genetic shackles
Surprisingly, the researchers observed that cortical thickness was not genetically determined. This independence from genetic determinants allows modifiable factors such as nutrition and exercise to have a favorable impact on brain health. It represents a ray of optimism, implying that lifestyle changes may play an important role in lowering dementia risk.
A non-invasive approach to dementia prediction
MRI’s simplicity and non-invasiveness make it a promising tool for predicting dementia. Claudia Satizabal, the study’s principal author, anticipates that “a person’s gray matter thickness might be analyzed as a percentile of the thickness of healthy people for that age.” This non-invasive metric has the potential to transform routine clinical practice.
Future frontiers: exploring modifiable factors and novel therapeutics
The future seems promising as the researchers investigate factors impacting cortical thinning, which include cardiovascular risk, food, genetics, and environmental contaminants. Modifiable factors may emerge as key contributors, changing our understanding of dementia risk and opening up new paths for therapies.
Clinical trials: identifying dementia in ‘on track’ participants
The newly discovered dementia ‘signature’ not only provides a possibility for early detection, but it also changes the landscape of treatment trials. Identifying participants ‘on track’ to develop dementia, even before symptoms appear, allows researchers to run more targeted and effective trials, bringing us closer to finding viable therapies.
Source study: Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association— A novel neuroimaging signature for ADRD risk stratification in the community